Injectable HIV medication: What you need to know
8 months ago | 75 Views
Long-acting, injectable medication is seen as a big advance in HIV prevention (PrEP) and treatment — an effective alternative to taking pills daily.
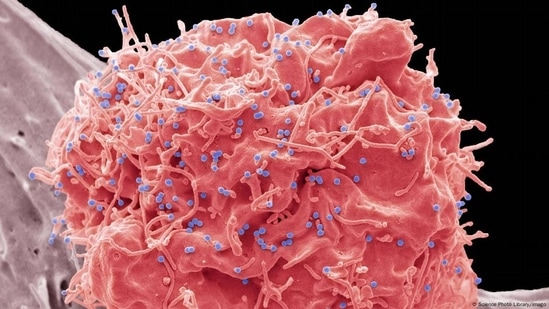
There's no vaccine for HIV, the virus that can lead to AIDS. And stories about people being cured of HIV are still read as miracles. HIV can, however, be prevented, controlled and treated with tablets — sold as Truvada.
But since 2020, Europeans living with the sexually transmitted infection have had an alternative to a daily regimen of pills: an injectable medicine.
The European Medicines Agency (EMA) approved rilpivirine and cabotegravir (sold as Rekambys and Vocabria, respectively, and together as Cabenuva). They are used in combination to treat patients with HIV-1, the most widespread type of the virus worldwide.
In 2021, the US Food and Drug Administration (FDA) approved cabotegravir (sold as Apretude) as a prophylactic. After an initial two doses, one month apart, people then take it every two months.
And in July 2022, the World Health Organization supported the use of long-acting injectable — cabotegravir (CAB-LA) — as a prophylactic.
HIV medicines 101: The difference between PrEP, PEP and ART
First, there are pre-exposure prophylaxis medicines, also known as PrEP.
PrEP is recommended for people considered at risk of infection. That includes, for example, people who inject drugs, including those in the chemsex scene (where drugs are used in group sex), certain ethnic groups (such as Blacks and Hispanics in the US), sex workers, and transgender women who have sex with men.
PEP, meanwhile, is also for people who don't have HIV but have had sexual contact with someone with HIV. PEP stands for post-exposure prophylaxis and is generally recommended in emergencies only.
And then there are treatments known as antiretroviral therapies, or ART.
ART helps people living with HIV lower their so-called "viral load" — the amount of HIV in their bodies — and supports their immune response.
The term "antiretroviral" is also abbreviated to ARV.
Why develop injections when we've got pills?
Until recently, PrEP, PEP and ART were exclusively available in pill form. And that has worked well, but at times people forget to take pills, some find it hard to swallow them, and others might feel stigmatized by having to carry pills around with them or keep them at home. Yet others might refuse to take them all together.
So, the hope is that long-acting, injectable medicines will "enhance treatment adherence, reduce stigma, and improve the overall quality of life for people living with HIV," said Meg Doherty, Director of Global HIV, Hepatitis and STIs Programmes at the World Health Organization.
"One of the most significant benefits of injectable HIV medication is the reduction in the pill burden. Instead of taking daily oral medications, individuals can receive injections in larger time intervals," said Doherty.
In 2022, the WHO said CAB-LA had been shown to be safe in two trials and resulted in a "79% relative reduction in HIV risk compared with oral PrEP."
Two years later, Doherty told DW: "If taken correctly, the efficacy of both long-acting injectable and daily oral ARV medications to suppress the virus are similar."
Doherty said that injectable medications may also have fewer gastrointestinal side effects compared to oral medications.
What are the disadvantages with injectable HIV medicine?
Long-acting HIV drugs have advantages and disadvantages.
"Dose frequency is still not ideal," said Doherty. "[They also have] complex injecting requirements — separate injections, intramuscular or intravenous route — and cold chain needs."
We've mentioned the two-month frequency for cabotegravir and rilpivirine. Another treatment drug, ibazulimab (sold as Trogarzo), is given every two weeks, either by injection or infusion. It needs to be taken in combination with other drugs.
Long-acting rilpivirine also needs refrigeration, which presents a potential limitation — it is potentially inconvenient for hotter climates and remote regions.
"Addressing these limitations is essential to ensure that injectable HIV medications can be effectively utilized in diverse settings," said Doherty.
Lenacapavir: An injectable only every six months
The drugs differ also in terms of what they target. Ibazulimab, for instance, is a monoclonal antibody — it's designed to behave like natural, human antibodies.
Lenacapavir, on the other hand, is a capsid inhibitor — the first of its kind in HIV treatment. It is designed to interfere with the HIV capsid, the protein shell that protects HIV's own genetic material.
[It's] the most promising," said Doherty. Lenacapavir only needs to be administered every six months — subcutaneously, just under the skin, and it doesn't require refrigeration.
But while data on cabotegravir and rilpivirine has been collected for four years now, there's still little data on long term efficacy and safety for lenacapavir — at least so far.
#